A cross-cultural research initiative led by the University of Waikato and Hiroshima University in Japan is advancing global understanding of how to build future-focused, equitable and climate-resilient health systems, with a strong focus on rural and ageing communities.

Dr Jesse Whitehead (centre, eighth from right) and colleagues from Te Ngira Institute for Population Research and the Division of Health alongside visitors from Hiroshima University.
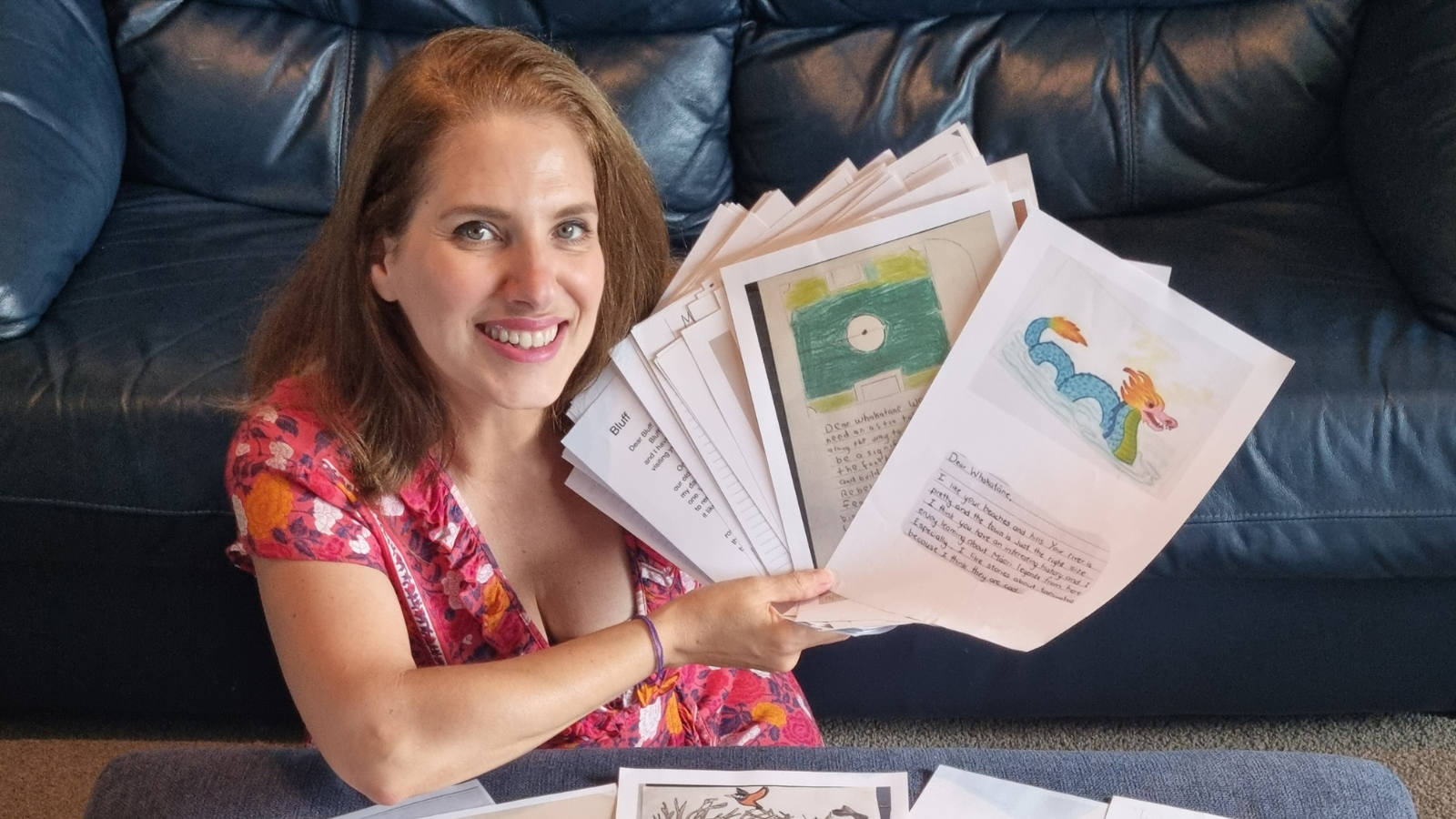
Dr Jesse Whitehead, Senior Research Fellow at Te Ngira Institute for Population Research at the University of Waikato, presented early insights and lessons from the collaboration at the recent National Rural Health Conference.
“We’re aiming to learn from each other’s strengths to help inform better health policy,” said Dr Whitehead.
“Japan is already a super-aged society, with well over 21% of its population aged 65 and over — a milestone New Zealand is expected to hit by the early 2030s.”
In late 2024, the Waikato research team visited Japan for on-the-ground insights into healthcare delivery and emergency response. A standout lesson came from the national Disaster Medical Assistance Team (DMAT) system. Unlike traditional models that wait for patients to reach hospitals, DMAT mobilises doctors, nurses, and emergency responders directly to disaster sites — speeding up treatment and saving lives.
“The level of preparedness is remarkable,” said Dr Whitehead. “Doctors and firefighters arrive on-scene together, enabling immediate triage and reducing preventable deaths. It’s a system New Zealand can learn a lot from.”
Dr Whitehead and his colleagues were also interested in the provincial scholarship system used to ensure a pipeline of doctors for rural areas.
“Each prefecture or region offered two students a scholarship to cover all costs for their medical degree, in return for a commitment to working locally. It’s an interesting model that works in their context.”
In a reciprocal exchange, researchers from Hiroshima University visited Waikato in early 2025 to explore New Zealand’s approaches to healthcare. They were particularly interested in chronic pain management, the role of general practitioners, and the culturally grounded principles that guide care delivery.
“In Japan, most patients see specialists directly when they’ve an immediate concern. Preventative medicine is predominantly done through annual medicals for all citizens during work time. The idea of having a GP as the first point of contact was unique to our guests,” said Dr Whitehead.
This ongoing collaboration is identifying strengths and gaps in each system with a view to policy impact. As both countries face rising healthcare inequities in rural regions, climate disruption, and ageing populations, the goal is to co-design practical solutions grounded in culture and community needs.
Dr Whitehead said he valued the chance to share more details with the National Rural Health Conference.
“By learning from each other, we’re creating pathways to more responsive, equitable, and resilient health systems — not just for Japan and New Zealand, but for rural and Indigenous communities worldwide.”